Our Pancreatic Cancer Foundation Is Making A Difference
The Seena Magowitz Foundation is a nation leader in pancreatic cancer awareness and care. Through initiatives like funding innovation pancreatic cancer research, we provide diagnosed patients as well as their family, loved-ones and caregivers with information to improve patient quality of life. Our Foundation shares the latest innovative research in cancer-care. To accomplish our mission we provide funding for pilot studies and clinical trials. Our primary focus is enhancing pancreatic cancer patient outcomes.
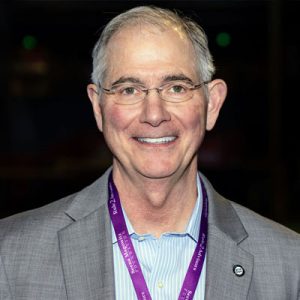
Survivor Stories
The Seena Magowitz Foundation’s “Pancreatic Cancer Patient Survivor Stories” page shares inspiring accounts of individuals who have battled pancreatic cancer. Recognized as a formidable and aggressive cancer with a stealthy onset, these survivor stories provide hope and insight into the challenges and victories faced by those affected. The narratives celebrate the resilience of survivors, many of whom have surpassed the five-year survival mark, defying the odds. These stories, drawn from diverse experiences, aim to offer encouragement and support to newly diagnosed patients and their families, highlighting the collective efforts of the cancer community, including research and oncology work.
Learn About The Pancreas
The pancreas is a crucial organ located behind the stomach and plays a dual role in the human body. It is divided into three parts: head, body, and tail. The pancreas performs two main functions: the exocrine function involves producing digestive enzymes that break down fats, carbohydrates, and proteins, while the endocrine function involves creating hormones, including insulin, to regulate blood sugar levels. These functions are vital for the proper digestion and metabolic regulation in the body. We also highlight some of the unique features of the anatomy of the pancreas, including the difficulty in detecting pancreatic tumors early due to the organ’s deep location within the abdomen, which can delay the diagnosis of pancreatic cancer.
Learn About Pancreatic Cancer
The Seena Magowitz Foundation’s page on “What is Pancreatic Cancer?” explains that pancreatic cancer involves the uncontrolled growth of abnormal cells in the pancreas, a gland that plays a key role in both the digestive and endocrine systems. There are two main types of pancreatic cancer: about 95% are exocrine tumors (pancreatic adenocarcinoma), which are highly aggressive with a low 5-year survival rate, and about 5% are endocrine tumors (neuroendocrine or islet cell tumors), which are generally less aggressive with a better prognosis. The page also distinguishes between benign (non-cancerous) and malignant (cancerous) tumors, noting that malignant tumors can metastasize, or spread, to other parts of the body.
Reducing Pancreatic Cancer Risk
The Seena Magowitz Foundation’s page on reducing the risk of pancreatic cancer offers practical advice for mitigating the disease’s risk. Key recommendations include avoiding smoking, maintaining a healthy weight, managing Type 2 Diabetes, staying vigilant for symptoms, and considering genetic testing if there’s a family history of cancer. Chronic pancreatitis, often linked to alcohol abuse, is highlighted as a risk factor. The page also addresses misconceptions, noting that pancreatic cancer can affect younger people too. Emphasizing vigilance, the page encourages regular communication with doctors and considering screenings for those at high risk. These measures collectively aim to lower the risk of developing pancreatic cancer.
Pancreatic Cancer Support Group
Other pancreatic cancer patients know what coping with pancreatic cancer is all about. They have navigated the same paths dealing with similar anxieties and obstacles. They share the same objectives. Our sole purpose in establishing this virtual support group is helping pancreatic cancer patients live life to the fullest extent. It is a dedicated approach focusing on patient wellness, hope, and inspiration. Helping our members heal and thrive in every respect. From the physical to the emotional and everything in between.