Causes and Differences Between Exocrine and Endocrine Pancreas Cancers
Video compliments of the National Pancreas Foundation
Written By Tony Subia
Dec 30, 2021
Pancreatic Cancer Introduction
Pancreas cancer has been linked to pancreatic diseases, including acute pancreatitis, chronic pancreatitis, and inflammation of the pancreas. While many people dismiss abdominal pain, those with a family history (or hereditary pancreatitis) should take further action when they experience these symptoms. Other risk factors, or indicators that there may be a case of pancreatic cancer, are cysts, gallstones, cystic fibrosis, or other pancreatic abnormalities. It is important to note that the most common causes of diseases of the pancreas, such as alcohol use, can also contribute to developing pancreatic cancer. Speak with your healthcare provider to see if you may be diagnosed with exocrine pancreatic insufficiency.
The pancreas is an important organ sitting behind your stomach. It’s like a little factory with two main jobs: one part makes juices that help break down food in the small intestine, and the other part makes hormones like insulin and glucagon that keep your blood sugar levels just right. Sadly, this organ can get two types of cancer. The more common type starts in the tubes (called ducts) where the digestive juices flow and is pretty serious. The other, less common type grows in the cells that make hormones and is usually not as tough to treat.
Doctors and scientists are always working to find these cancers early and treat them better. They use special tools to look inside the body, like tiny cameras on tubes (endoscopy) or tests that take pictures of the inside of your body (like ERCP, which looks at the pancreatic duct, gallbladder, and bile duct). They also use blood tests to find clues about what’s going on. If someone has pancreatitis, which is when the pancreas gets inflamed, it can be because of a blockage or something wrong with the immune system. Sometimes, the doctors have to do surgery, called a pancreatectomy, to fix the problem or help with the pain. Organizations like the National Pancreas Foundation are there to help people understand more about these problems and how to deal with them.
The Pancreas Performs Two Different Functions.
So There Are Two Main Types of Pancreatic Cancer.
In the intricate landscape of human physiology, the pancreas plays a dual role, functioning both in the digestive system and the endocrine system. This multifunctionality of the pancreas leads to the existence of two main types of pancreatic cancer, each corresponding to the distinct functions of the organ. The first type originates from the cells involved in digestive functions, targeting the exocrine component, which is more common and includes adenocarcinomas. The second type arises from the endocrine part of the pancreas, which is responsible for regulating blood sugar levels through hormone production, leading to a rarer form of cancer known as neuroendocrine tumors. Understanding this dual nature of the pancreas is essential for comprehending the complexities of pancreatic cancer, guiding both diagnosis and treatment strategies.
Like all organ and tissue cancers, pancreatic cancer is caused by gene mutations which causes pancreas cells to multiply uncontrollably. They will continue to live whereas normal cells will die. As uncontrolled, abnormal cancerous pancreas cells multiply, they bond together to form a malignant tumor. The tumor will continue enlarging as the abnormal cells continue to multiply.
According to Johns Hopkins Medicine, it takes at least 10 years for the first pancreatic cancer cell within a pancreatic lesion to turn into a full-fledged cancer cell. It can take about an additional 7 years after the first cancer cell appears to multiply into billions of cancerous cells to form a malignant tumor the size of a plum.
Understanding Pancreatic Cancer: The Exocrine and Endocrine Roles
The pancreas is an organ with two key roles crucial for our well-being. The exocrine part of the pancreas churns out digestive enzymes, which break down food into nutrients in the digestive tract. Meanwhile, the endocrine section produces vital hormones, such as insulin and glucagon, which work in tandem to regulate the glucose levels in our blood.
A staggering 90% of pancreatic cancers start in the exocrine part, in the cells lining the pancreatic ducts, leading to what is known as pancreatic adenocarcinoma—recognized as the most common and lethal form of pancreatic cancer. In contrast, the endocrine part can develop pancreatic neuroendocrine tumors, a rarer type of cancer accounting for less than 5% of cases and typically exhibiting a less aggressive nature.
The Development and Characteristics of Pancreatic Cancer
As highlighted by the National Cancer Institute (NCI), pancreatic cancer is a complex disease that starts from mutations in the cells of the pancreas. These mutations disrupt the normal cell cycle, leading to uncontrolled multiplication and the formation of a malignant tumor. This tumor can continue to grow as abnormal cells proliferate.
Exocrine Pancreatic Cancer: The Dominant Threat
The exocrine pancreas plays a crucial role in digestion, producing enzymes that break down carbohydrates, fats, and proteins. However, it’s also the site where over 90% of pancreatic cancers originate. These cancers, primarily adenocarcinomas, start in the ducts of the pancreas. Exocrine pancreatic cancers, including duct cell carcinoma and acinar cell carcinoma, exhibit aggressive behavior and poor prognosis. The overall survival rate is less than 6%, and curative treatments are rare, especially since most cases are diagnosed at an advanced stage.
Johns Hopkins Pathology states that cancer of the pancreas is not a single disease but encompasses up to ten different tumor types under the umbrella term “cancer of the pancreas.” Each tumor type requires a specific treatment approach and carries a unique prognosis, emphasizing the importance of accurate diagnosis for effective management.
Endocrine Pancreatic Cancer: A Rare but Manageable Condition
In contrast, pancreatic neuroendocrine tumors (NETs) form in the hormone-producing islet cells of the pancreas. Accounting for less than 5% of all pancreatic cancers, these tumors can be either functional, producing excess hormones like insulin, gastrin, and glucagon, or nonfunctional, showing no such hormonal activity. Functional NETs lead to conditions like insulinoma, gastrinoma, and glucagonoma, each associated with specific symptoms depending on the excess hormone produced.
The prognosis for pancreatic NETs is generally more favorable than exocrine pancreatic cancers. The cure and survival rates vary based on factors like the type of tumor, its location in the pancreas, whether it has spread, and the patient’s overall health.
Risk Factors and Diagnosis
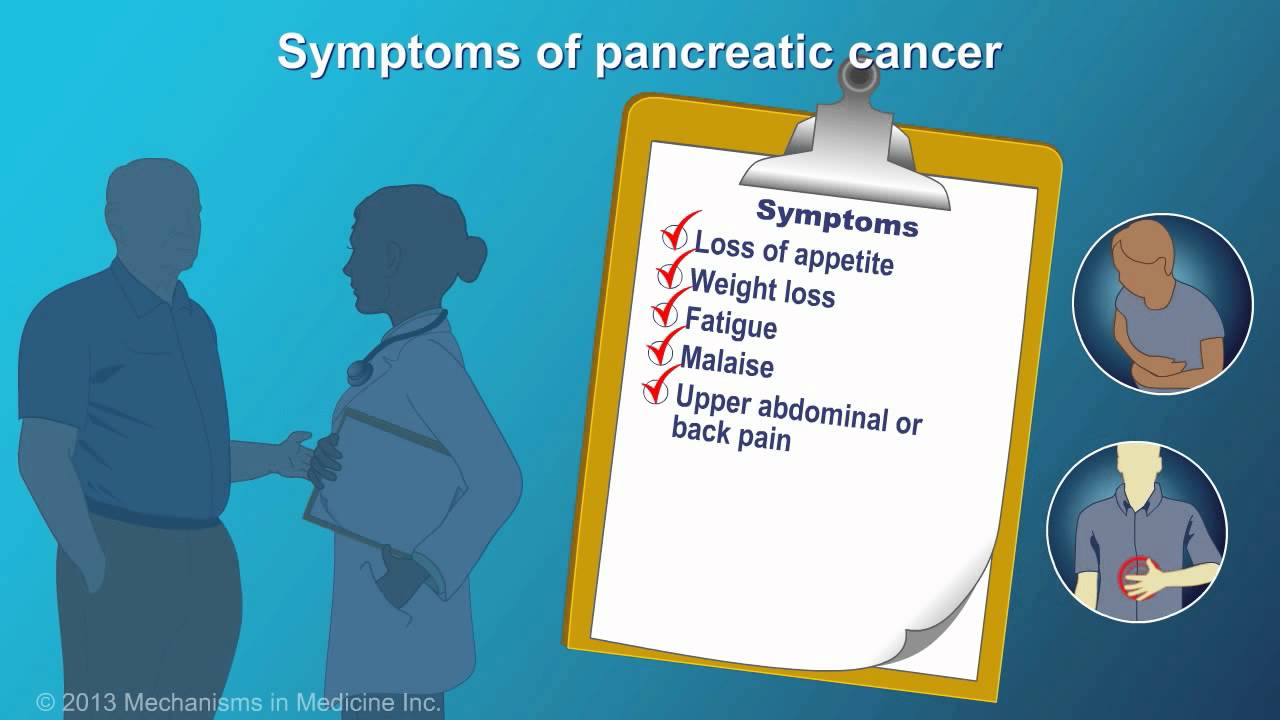
Risk factors for pancreatic cancer include genetic predisposition, lifestyle factors such as smoking, and certain chronic conditions like diabetes and pancreatitis. Early detection remains challenging due to the pancreas’s deep location in the abdomen and the often-silent nature of the symptoms in the early stages of the disease.
Diagnostic methods for pancreatic cancer involve a combination of laboratory tests, imaging techniques, and sometimes biopsy. For exocrine pancreatic cancers, imaging tests like CT scans and MRIs are crucial in identifying the extent of the disease and guiding treatment planning.
Current Treatment Approaches
Treatment for pancreatic cancer is highly individualized, depending on the type and stage of the cancer. For exocrine pancreatic cancers, surgical resection offers the best chance for a cure but is only viable in a small percentage of patients with localized disease. Chemotherapy and radiation therapy are used in more advanced cases or to shrink tumors before surgery.
For endocrine pancreatic cancers, surgical removal of the tumor is often possible, especially for functional NETs, which are usually localized and slow-growing. Medical therapies for NETs include targeted therapies and hormone therapy to manage symptoms and control tumor growth.
Research and Future Directions
Research in pancreatic cancer is ongoing, with a focus on understanding the genetic and molecular mechanisms underlying the disease. This research is crucial in developing new treatments and improving early detection methods. Clinical trials are continually exploring innovative treatment strategies, offering hope for more effective management of this challenging disease.
In conclusion, while pancreatic cancer remains a formidable health challenge, advancements in research and treatment are providing new insights and hope. Understanding the differences between exocrine and endocrine pancreatic cancers is key to developing targeted and effective treatment strategies.
Advanced Diagnosis and Treatment Options
Advancements in diagnostic technologies have significantly improved the ability to detect pancreatic cancer. Techniques like endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP) allow for detailed visualization of the pancreas, aiding in early diagnosis. For exocrine pancreatic cancers, these imaging tests are essential for staging the cancer and planning treatment.
The treatment for exocrine pancreatic cancers often involves a combination of surgery, chemotherapy, and radiation therapy. The Whipple procedure is a common surgical technique used for tumors located in the head of the pancreas. However, due to the aggressive nature of these cancers, many patients also require chemotherapy and radiation to manage the disease.
In the case of endocrine pancreatic cancers, treatment options include surgical removal of the tumor, targeted therapy, and hormone therapy. These cancers often respond well to treatments, especially when detected early. For functional NETs, surgery is the primary treatment to remove the hormone-producing tumor.
Challenges and Ongoing Research
Despite advancements, pancreatic cancer remains one of the most challenging cancers to treat. Its late presentation, aggressive nature, and resistance to treatment contribute to its high mortality rate. Ongoing research is focused on understanding the molecular and genetic basis of pancreatic cancer to develop targeted therapies. Clinical trials exploring new chemotherapy drugs, targeted therapies, and immunotherapies are underway, offering hope for improved outcomes.
Researchers are also investigating early detection methods, including biomarkers in the blood that may indicate the presence of pancreatic cancer. These efforts aim to identify the disease at a more treatable stage, potentially improving survival rates.
Living with Pancreatic Cancer
Living with pancreatic cancer can be challenging, both physically and emotionally. Patients often require support from a multidisciplinary team, including oncologists, surgeons, nutritionists, and mental health professionals. Managing symptoms, maintaining nutritional health, and coping with the emotional impact of the disease are critical aspects of care.
Support groups and patient advocacy organizations offer resources and community support, helping patients and their families navigate the complexities of the disease.
Moving Forward With Pancreatic Cancer
There are many signs and symptoms that you may be dealing with pancreatic cancer, including jaundice, unexplained weight loss, and autoimmune disorders. In addition, a history of a specific cause of pancreatitis, such as pancreatic cysts, pseudocysts, or disorders of pancreatic enzymes, are signs that you may be dealing with something more serious.
Pancreatic cancer, whether exocrine or endocrine, poses significant challenges in terms of diagnosis, treatment, and patient care. While the prognosis for exocrine pancreatic cancer remains poor, advancements in treatment and research offer some hope. For endocrine pancreatic cancers, the prognosis is generally more favorable, especially with early detection and appropriate treatment.
As research continues to unravel the complexities of pancreatic cancer, there is cautious optimism that future breakthroughs will lead to more effective treatments and improved survival rates. Understanding the nuances of both exocrine and endocrine pancreatic cancers is crucial for developing tailored treatment strategies and providing the best possible care for patients.
This article discusses what causes types of pancreatic cancer and the dual roles of the pancreas including the Exocrine and Endocrine functions of the pancreas. The information is only provided for educational purposes only. It is not intended to replace professional medical advice. Always consult with your medical providers for medical advice.